Clover Health Data Report Finds Neighborhood Determines Health Outcomes
Report Analyzes the Disparity Divide
Overview
Clover Health cares deeply about providing quality healthcare to all Medicare-eligible seniors, especially minorities and low-income individuals residing in communities that have historically been excluded from the benefits of Medicare Advantage (MA) plans. To best serve those most in need, it's imperative to consider the socioeconomic barriers associated with the neighborhoods in which marginalized populations live as we treat patients, measure impact, and evaluate health plans. Without understanding existing disparities, policymakers risk creating metrics that reinforce or exacerbate inequity.
Using the Area Deprivation Index (ADI)—a Census-based measure derived from income, education, homeownership, and household status—to quantify location-based, socioeconomic determinants and layering on Clover's proprietary clinical data, we are able to see the impact that socioeconomically disadvantaged neighborhoods have on a person's health outcomes. Previous studies have identified the correlation between higher-cost Medicare beneficiaries and such disadvantaged neighborhoods, and Clover’s data supports these findings while also providing additional details related to metrics in the MA Star Ratings Program that the Centers for Medicare & Medicaid Services (CMS) uses to evaluate MA plan performance. Because the Star Ratings Program fails to take into account the impact of geographic locale on member outcomes, these findings demonstrate that CMS ultimately penalizes plans that serve members residing in socioeconomically disadvantaged neighborhoods.
Results
Management of chronic diseases
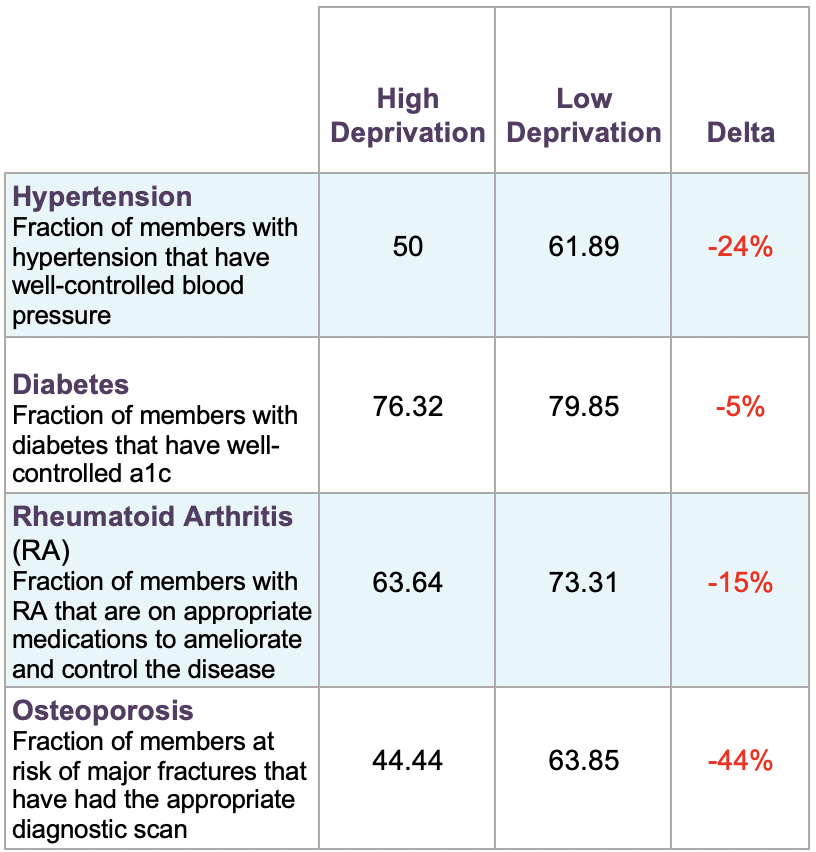
Proper management of chronic diseases is essential for the Medicare population. Of older adults, 85% have at least one chronic disease, and 60% have at least two. The data shows that Clover patients residing in areas with a higher area deprivation index (ADI) were significantly less likely to be properly managing their chronic conditions such as diabetes, arthritis, and hypertension.
The largest disparity showed that members from high-deprivation areas are 44% less likely to have diagnostic scans completed for osteoporosis, a common cause of hip fractures in older adults. Breaking a hip creates a decline in mobility and independence for seniors, and the mortality rate within the first year of a bone break is 33%.
Undiagnosed Diseases
Clover found that individuals from high-deprivation areas are not only less likely to be properly managing their diagnosed chronic diseases, but also 15% more likely to be suffering from undiagnosed disease burden.
Clover Health uses advanced machine learning (ML) data models to surface potential diseases directly to doctors to help them identify the additional conditions that might bear on the treatment and health of their patients. Since the company has access to each member's history of medications, procedures, lab test results, diagnoses, and screening scores and symptoms from the member’s interactions across the healthcare ecosystem, Clover is able to construct a holistic health profile of each member. ML models identify specific undiagnosed conditions that the individual might have and surface that information directly to doctors through the Clover Assistant platform. The doctors review that information, use their own clinical judgement to determine if their patients are suffering from a disease, and then take the appropriate steps to implement a care plan. The models are built with tight feedback loops, so every time the doctor confirms or rejects a suspected diagnosis, it improves the accuracy of the model.
Tuning the models with clinical verification directly from hundreds of primary care doctors has allowed Clover to assist physicians in successfully identifying, diagnosing, and implementing care plans for thousands of diseases in Clover’s membership.
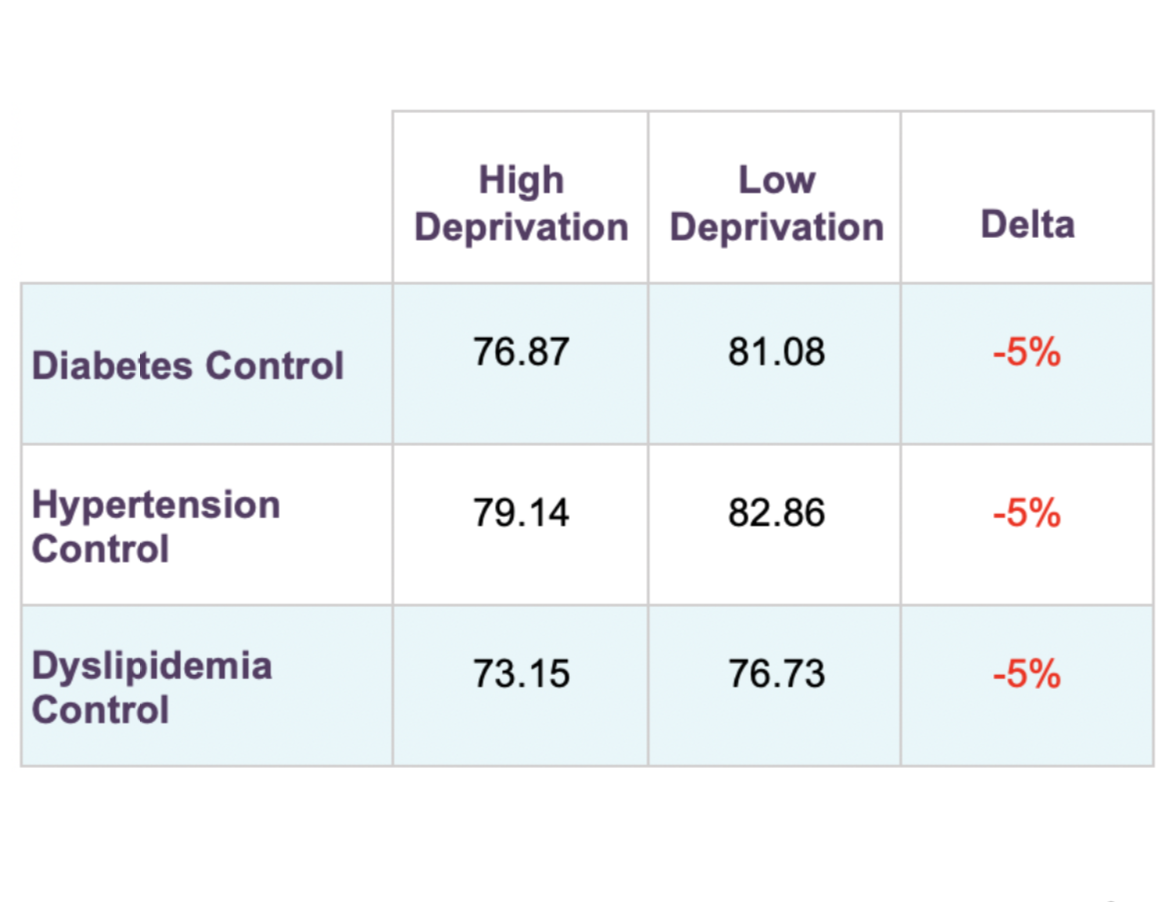
Medication Adherence
For all patients, and seniors especially, with chronic diseases, sticking to a regimen of prescribed medications is vital to successful disease management. Across diabetes, hypertension, and high cholesterol patients, members in high-deprivation areas have lower medication adherence, which puts them at higher risk of suffering an acute health event.
Two hypotheses for low rates of medication adherence among lower-income Medicare Advantage members are that they don't have the expendable income to afford their co-pays every month and they are unable to physically get to the pharmacy. While 100-day scripts and medication delivery services help reduce these barriers, they still exist within Clover's membership and across the Medicare population.
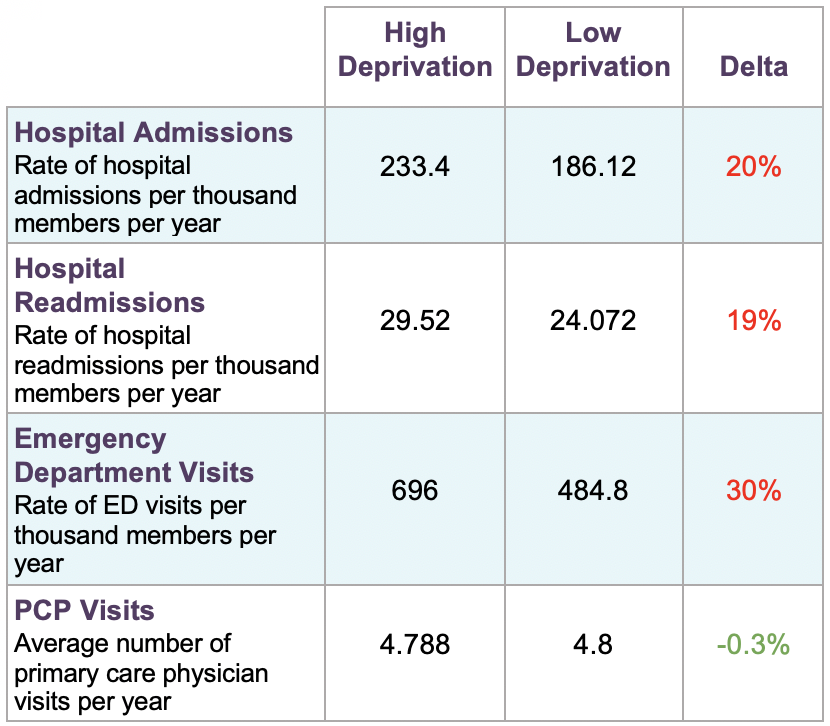
Acute Health Events
Clover members from high-deprivation areas visit hospital emergency departments 30% more frequently than those from low-deprivation areas. It has been cited that lower-income individuals tend to use the hospital over primary care because emergency departments don't have co-pays, and this appears to hold true for Clover's members coming from socioeconomically disadvantaged neighborhoods, regardless of income.
Clover has specifically developed its plans to have zero-cost, primary care physician (PCP) and low specialist copays to curb this behavior and has seen success—with both high- and low-deprivation members seeing their PCP at a nearly equal rate. However, high-deprivation patients still visit the emergency department at a higher rate, likely due to the mismanagement of chronic diseases and poorer medication adherence indicated above.
Conclusion
Across the board, Clover members from higher deprivation areas had chronic diseases less under control; poorer adherence to medications; and more frequent emergency department visits, hospitalizations, and hospital readmissions. It's clear that Medicare beneficiaries from underserved communities face greater socioeconomic barriers than beneficiaries from less disadvantaged areas, and those barriers adversely impact their health outcomes. While Medicare Advantage plans serving these communities must help members address those challenges, the MA Star Ratings Program completely overlooks the systemic disparate impact of the socioeconomic status of a member’s neighborhood on health outcomes. We note that while CMS takes member eligibility for the Medicare Low Income Subsidy (LIS) into consideration for Star Ratings, our data shows that an individual's geography has a far greater impact than does LIS-eligibility on members’ management of chronic diseases, their adherence to medications, and the proper assessment of their disease burden.
Unfortunately, the way the Star Ratings Program's quality bonus payments are designed today reinforces and exacerbates the existing health disparities between socioeconomically advantaged and disadvantaged communities. Such disproportionate outcomes do not align with CMS’s critically important goal of advancing health equity across the Medicare-beneficiary population. In order to address the health needs of America's aging population effectively, policymakers need to consider all aspects of health, including geographic factors, and align incentives for Medicare plans to serve those needs. Otherwise, we risk perpetuating the cycle of patients living in high-deprivation areas having fewer and lower-quality healthcare options solely due to their socioeconomic circumstances.
Clover proudly embraces serving a diverse population of members, many of whom reside in high deprivation areas. We do this because we believe in improving every life. We're committed to our members, both present and future, and will continue digging into our data to understand where we, and the industry as a whole, can provide better care for all Medicare beneficiaries, including the most vulnerable.
Methodology
The insights in this report were collated using an analysis of Clover Health's proprietary data, paired with publicly available Area Deprivation Index (ADI) data. Clover has integrated ADI data into its platform because the company repeatedly sees the impact neighborhood socioeconomic status has on outcomes, and understanding the barriers individuals face allows us to deliver more impactful clinical programs. Clover proudly serves many low-income and often overlooked communities, which is core to the company's mission of bringing healthcare to individuals and communities that are most in need and are commonly bypassed by other MA insurers.